
 Getty Images
Getty Images
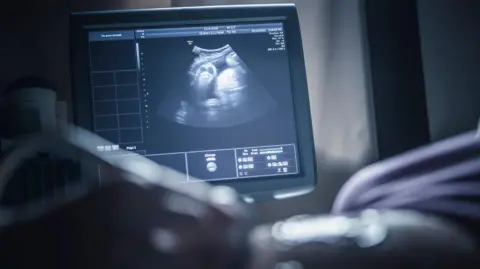
Pregnant women in Northern Ireland face discrimination over not being offered early screening for foetal abnormalities, according to gynaecology experts.
Early screening for the likes of Patau, Edwards’ and Down’s syndrome, are routine in the rest of the UK.
Several patients, who contacted BBC News NI, described the trauma they experienced after their “non-viable” pregnancies were not detected until about 20 weeks.
In Scotland, Wales and England antenatal screening which tests for anomalies is offered to all pregnant women in the first trimester – between 11 and 13 weeks.
The Royal College of Obstetrics and Gynaecology (RCOG) said women in Northern Ireland have foetal abnormalities diagnosed “too late” and should not have to wait until their 20-week scan.
What is first trimester screening?
It is an initial screening test, combining a blood test and an ultrasound scan.
It indicates a high likelihood for the foetus to be affected by one of the three conditions namely Patau, Edwards’ and Down’s syndrome.
Women affected will then be offered either further screening involving a blood test called the Non-Invasive Prenatal Testing (NIPT) or an invasive diagnostic test such as amniocentesis.
Alternatively, a woman may choose to have no further testing.
One couple’s ‘lonely’ journey
One couple said they opted for a termination after the foetus was diagnosed with several anomalies at their 20-week scan.
The woman was, in fact, more than 21 weeks pregnant before she could be treated.
The couple, who have asked for their identities to be protected, said it was such a “lonely time that they wish on no-one else”.
Sarah, not her real name, said family and friends believed she miscarried at 20 weeks.
“We did not feel comfortable telling family and friends about the horrendous situation we had found ourselves in, and the impossible choice we had to make for fear of being judged.
“Choosing to end a very much wanted pregnancy is a horrendous situation to be in and an unthinkable choice no matter how far along you are.
“We believe had we been in the position to do so earlier in the pregnancy it would have been a lot less traumatic both emotionally and physically.”
She added that ending a pregnancy brings on “mental torture that babies born within the second trimester can and do survive”.
‘I was clearly pregnant’
Another woman, Emily – not her real name – said it had been “devastating” that she could have known about the “fatal anomaly” earlier.
“The lack of screening meant we were allowed to believe everything was fine and sleepwalk into a situation where I was clearly pregnant to all of those around me,” she said.
“It was not until a year after our loss that we learned there was a discrepancy between the care in Northern Ireland and mainland UK,” said Emily.
At 21 weeks pregnant, Emily said the only option available was to be medically induced into labour to terminate a non-viable pregnancy.
“As someone who had never given birth before, it was traumatic, painful, and scary in those circumstances.”
She added: “Being given no option but labour at 21 weeks is a different proposition entirely to being given the sad news with options at 12 weeks.”
‘Physical and mental well-being’


A new framework for abortion services in Northern Ireland drawn up by the Northern Ireland Office took effect in March 2020.
It also means no time limit for terminations when there is a “substantial risk” a foetus would suffer a severe mental or physical impairment.
The RCOG has called for earlier scans, with some medics arguing women in Northern Ireland are being “discriminated against”.
Dr Caitriona Monaghan, a consultant in maternal foetal medicine, said late diagnosis at the 20-week scan affects how women choose to manage their pregnancy.
Dr Monaghan, who is member of the ROCG, said: “It limits access to care, including palliative care; it limits what decisions they can make and, as it comes at a later stage in their pregnancy, it puts them under time pressure to make decisions.
“It also affects a woman’s physical and mental well-being.”
Dr Monaghan added that screening is not only about the screening of genetic conditions.
“It’s about screening for important conditions such as preeclampsia which can affect both mums and babies from an early stage in pregnancy,” she added.


Dr Fiona Bloomer from Ulster University said there is still a lot of stigma in Northern Ireland around abortion which prevents couples and families talking openly about their experience.
Dr Bloomer, who has been involved in academic research on foetal abnormalities, said the main stumbling block is funding earlier screening.
“I am hopeful that the Department of Health will take a stance, I think they will see the need for earlier screening to be made available – the issue will be when they commit the budget to it,” she said.
The Department of Health confirmed official guidance in Northern Ireland meant scans for detecting abnormalities were only carried out during the second trimester.
The department said work is “ongoing” on how much and how long is required to introduce recommendations on “first trimester antenatal screening for foetal anomalies and inherited conditions”.
It added that once the information is collated it will be considered by the Northern Ireland Screening Committee before future policy decisions can be made.








