Key questions that remain about Nottingham killer’s care

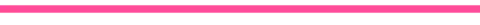
 Nottinghamshire Police
Nottinghamshire Police
The critical report into the mental healthcare given to Valdo Calocane – a paranoid schizophrenic who fatally stabbed three people in Nottingham last year – is damning.
In the lead-up to the attack, mental health assessments document how he often stopped taking his medication and was showing increasingly violent behaviour. But despite these red flags, the risks he posed were minimised and there was a “series of errors, omissions and misjudgements”, the Care Quality Commission (CQC) found.
Calocane was suffering paranoid delusions when he killed Barnaby Webber, Grace O’Malley Kumar and Ian Coates. Their families say the failings exposed in the report are even worse than they previously thought, and have been told there will be a public inquiry.
At the centre of the criticism is the Nottinghamshire Healthcare NHS Foundation Trust (NHFT), which says it accepts the findings of the report and is working to improve its services.
But several key questions remain about Valdo Calocane’s care.

 Family Handout
Family Handout
Could more have been done to ensure Calocane took his medication?
Yes, there are circumstances in which mental health patients, who are very ill, can be forced to take medication.
The CQC report details how over the two years that Calocane was being treated by NHFT, he often stopped taking his medication.
Out-of-date tablets, which were the main treatment for his paranoid schizophrenia, were found in his flat.
He also missed multiple appointments with mental health teams, and his medical records chart his increasing violence as he became acutely unwell.
Given this pattern of behaviour, the report says he could have been given what are known as depot injections – these deliver long-lasting medication – but Calocane consistently refused this.
Mental health staff do have to work with patients, balancing their wishes and rights with the need to ensure they get necessary treatment.
But stronger powers can be used.
Each time Valdo Calocane reached a crisis he was detained under Section 2 of the Mental Health Act. But if Section 3 had been used, clinicians could have insisted he had depot injections.
This would also have allowed him to be given a Community Treatment Order (CTO), meaning he would have been more closely supervised in the community. Under a CTO, if a patient stops taking their medication or misses too many appointments, they can immediately be recalled to hospital.
The CQC concludes “these would have been important components in a more robust package of care for Valdo Calocane”.
Could more have been done to involve Calocane’s family?
Yes, and his mother and brother, who lived many miles away, say they tried to raise concerns about his deteriorating mental health.
But they say they felt shut out by professionals who didn’t always listen to them, and by the rules on confidentiality, which limited what Calocane’s closest relatives were told.
The family told BBC Panorama that by early 2022, Calocane had told his mental health team that he did not want information shared with them.
Many families argue that they know their loved ones best and can provide important insight into how an illness is affecting that person, and pick up on warnings when they are deteriorating.
Calocane’s family were not alone in this experience – the CQC report says it looked at other cases in Nottinghamshire, and found more families who also felt excluded from the care of their mentally ill relatives.
The laws on patient confidentiality are the same for mental health patients as for anyone else, with a few exceptions.
The Mental Health Act Code of Practice says there are circumstances “in which it is both justifiable and important to share otherwise confidential patient information with people outside the immediate team treating a patient”.
That includes to protect others from harm or to prevent serious crime.
With hindsight it is easy to make a case for more information being shared in this situation, but the mental health teams did not have that.
However, the CQC report says: “It could be argued that the Trust could have continued to engage with the family while still maintaining his confidentiality.”
It also says “We can see that efforts to engage him assertively and to liaise with his family reduced notably” from April 2022 when his care moved to a new mental health team.


Were pressures on mental health services a factor?
We know that across the UK mental health services are under huge pressure, but we do not know how much impact that had on this case.
Although mental health funding has increased, it has not kept up with the rising demand.
The most up-to-date NHS figures show that in June this year 1.94 million people were in contact with mental health services in England – an increase of more than 30% in three years.
There are also significant staffing shortages. According to the King’s Fund think-tank, in September last year there were 28,600 staff vacancies in mental health – about 19% of the total workforce.
Those pressures form the backdrop to Valdo Calocane’s treatment.
In March, the CQC published a rapid review which said it had been raising concerns about mental health services in Nottinghamshire for five years.
It highlighted staff shortages and long waiting lists for services. The review also identified problems finding enough beds for people who needed inpatient treatment, which then had a knock-on effect for other services.
The review said community-based teams were having to manage more complex and acutely ill patients.
“This created greater risk and pressure on community teams, whose therapeutic input lessens as they manage increasing levels of crisis,” it found.
The latest CQC report looking specifically at Valdo Calocane’s care points to staff shortages in some of the teams he was seeing.
What happens next ?
An NHS report into the case is due soon, and that may provide a clearer picture of how much pressure services were under.
There are also ongoing inquiries into how the police handled incidents involving Calocane.
But the families of those who died believe only a public inquiry can draw together all the threads to provide the answers and change that they want.
They say individuals and organisations must be held to account, and have been told that the public inquiry they have been calling for will happen.
Nottinghamshire Healthcare NHS Trust said its thoughts were with “all those whose lives changed irreparably after the attacks”.
It also said it accepts the conclusions of the CQC reports and has “significantly improved processes and standards” since Calocane’s assessments were carried out.